BA.2 is evading protections like masks and vaccines, but experts say it’s not time to abandon precautions

Figuring out where you’re most at risk of catching COVID-19 is more challenging than ever in Canada’s Omicron-fuelled sixth wave, and tried-and-tested strategies for avoiding infection are proving less effective in everyday life.
The rapidly spreading BA.2 subvariant has been evading all of our layers of protection — from vaccines to masks — and fuelling a surge of COVID-19 levels across Canada during a time of few restrictions.
But while attempting to avoid COVID-19 risk entirely isn’t realistic, abandoning strategies that have worked to lessen the impact of the virus isn’t either — making this phase of the pandemic incredibly difficult to navigate.
“We have not experienced what it’s like to live with this virus while we are doing this little to stop it,” said Dr. Jeremy Faust, an emergency room physician at Brigham and Women’s Hospital and a Harvard Medical School instructor who recently wrote about navigating risk.
“Never until now have we been in a situation in which we have the least amount of protection against infection and these variants that are just flabbergastingly contagious.”
Hard to judge, hard to avoid
Faust says because everyone has a different risk threshold in day-to-day life, trying to navigate the pandemic based on your presumed best interest is a “dead end” because many people are unlikely to have judged the situation correctly.
“We might be completely correct one day and be safe and be completely incorrect the next day and be either personally at risk or putting someone else at risk,” he said. “And it’s this variability that makes your head spin if you stop to think about it.”
Dr. Lynora Saxinger, an infectious diseases physician and associate professor at the University of Alberta in Edmonton, said part of the problem with Omicron is that it punches through all our layered protections “much more effectively than anything has before.”
“All of those layers still reduce your risk, it’s just that the assault on the layers is a lot more aggressive right now,” she said. “It’s like there’s a lot more shots on goal.”
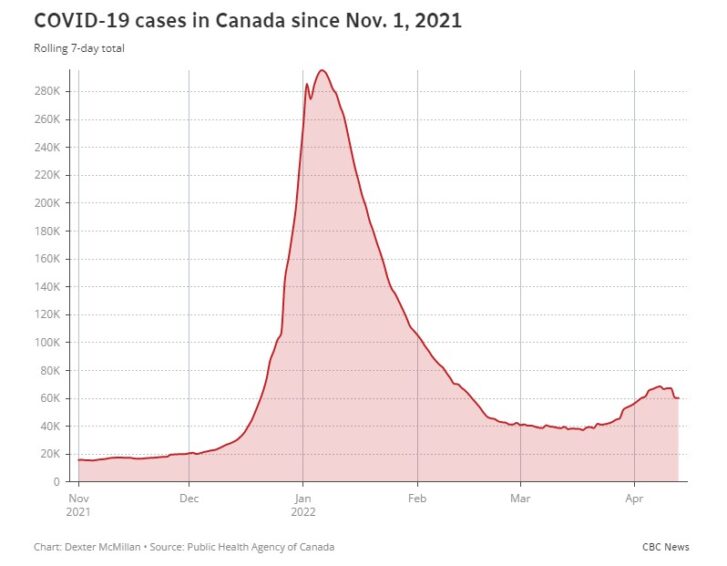
Saxinger said that even though Canada is vastly undercounting current case numbers there is still a “forest fire of COVID” raging across the country, with transmission signals recently rising in Alberta, Ontario, Nova Scotia, Saskatchewan and Manitoba despite limited testing.
“The risk of infection has gone up markedly over the past three months,” said Erin Bromage, an associate biology professor at the University of Massachusetts Dartmouth who researches infectious diseases.
“And it’s getting harder for those who have avoided infection up until now to continue avoiding infection.”

Playing field ‘rapidly shifting’
Canada’s Chief Public Health Officer Dr. Theresa Tam said this week that average daily case counts, test positivity rates and wastewater signals are all signalling growing transmission across the country that requires the “layering of precautions” to drive infection rates down.
“There is still a lot we can do to dampen down the current trajectory,” she said during a press conference Wednesday.
“We know that using personal protective measures like masking helps reduce transmission. Likewise getting a booster dose doesn’t just protect you against severe illness, it also provides a level of protection against infection.”
But the effectiveness of masking in preventing the transmission of Omicron and its highly contagious subvariants isn’t perfect, and the protection against infection from boosters appears to be waning at a rapid rate.
Linsey Marr, a researcher on the airborne transmission of infectious diseases and a professor at Virginia Tech says that while masks have the same filtration level for any virus — our chance of infection could be higher with these more transmissible variants.
“One thing that might be different with the variants is that people could be shedding more virus into the air…. You’re exposed to more virus, so your chances of infection are higher,” she said. “Another thing that might be different is that the infectious dose could be lower.”
Marr said there seems to be a “significant change” with masks against Omicron and its subvariants, meaning a cloth mask that may have been somewhat protective before is no longer sufficient and that higher-quality masks may be necessary.
“The masks could help blunt it a little bit, but they weren’t going to stop this wave or prevent this wave from happening,” said Dr. Isaac Bogoch, an infectious diseases physician and member of Ontario’s COVID-19 vaccine task force.
“I’m very much in favour of indoor masking, I’m very much aligned with ‘the mask mandate should not have been lifted,’ but it would not have stopped or prevented this wave.”WATCH | Canadians urged to get booster shots to blunt 6th wave:
All signs indicate Canada is going through a sixth pandemic wave, Dr. Theresa Tam confirms. Her message to Canadians: wear a mask and get boosted if eligible.
Additional booster doses of the vaccine are also beneficial in preventing severe disease across the population, but a large new Israeli study in the New England Journal of Medicine showed fourth-dose protection against infection waned after just four weeks.
The observational study focused solely on adults aged 60 and older and found protection against severe illness didn’t wane in the six weeks after a fourth dose, but the data was too limited to determine whether a second booster provided better long-term protection.
“I’m not surprised that fourth doses aren’t generating very durable protection against infection,” said Dr. David Naylor, who led the federal inquiry into Canada’s 2003 SARS epidemic and now co-chairs the federal government’s COVID-19 Immunity Task Force.
“Two shots were much more effective against Delta. What’s clearly changed is that two or even three shots won’t preclude getting any of the substrains of Omicron.”
Naylor said fourth doses make sense for elderly Canadians, the immunocompromised and those with comorbidities, adding that we should be cautious with Israeli data because of the different spacing of doses there and their sole reliance on the Pfizer vaccine.
“We also have lots more people now with hybrid immunity — one, two or three shots, plus an infection in the last few months that may be increasing their level of protection,” he said.
“It’s a rapidly shifting playing field.”
Worth delaying infection if possible
So while avoiding COVID-19 infection may not be feasible for most people, delaying it until you’re as protected as possible has benefits — and there are still ways you can lessen risk.
“To try and avoid infection, people still need to avoid indoor spaces that are crowded or that create close contact,” said Bromage, who wrote a viral blog post in May 2020 shared by millions explaining the places people are most at risk of COVID-19 infection.
“When in those situations, people need to wear higher quality masks than they used previously — preferably N95 or equivalent — and limit the time in those spaces. Duration matters.” WATCH | Why the rollout of third doses of COVID vaccine has stalled:
Confusion over when to get third dose of the COVID-19 vaccine after having the virus and complacency over loosened restrictions have stalled uptake of booster doses in Canada.
Increased immunity, broader availability of COVID treatments and two years’ worth of knowledge among members of the medical community are also helping to ensure that when people do get sick, they’re getting the best possible care.
It’s still a crisis, but the situation in Canada and abroad is steadily improving, stressed Bogoch.
“I’ve spoken with people in their 80s, who are triple vaccinated, who got COVID… but who are going to recover from this infection without having to come to a hospital. That’s amazing,” he said.
“Before the vaccines were available, many of these people would have gotten very sick, landed themselves in hospital, needed an intensive care unit and many would have died.”
In Italy, one of the countries hard hit by COVID-19 early on in the pandemic — with one of the highest global death tolls — new research suggests vaccination efforts roughly halved the number of deaths.
Vaccines prevented some 150,000 fatalities last year, the country’s National Health Institute (ISS) estimated on Wednesday, as well as more than 500,000 hospitalizations and over 55,000 admissions to intensive care.
Focus on being ‘maximally vaccinated’
Even though it’s tough to avoid catching COVID, it’s worth buying time if you can while the scientific community develops and approves drugs and treatments that could cut that risk even further, said Dr. Abraar Karan, an infectious diseases fellow at Stanford University in Stanford, Calif.
“The fact that they now have more knowledge in terms of how to treat COVID means that when they do have these big surges, there are tools that they can use to reduce the infection fatality rate,” he said.
Just this week, Health Canada authorized AstraZeneca’s antibody-based therapy for preventing COVID-19 infections for immunocompromised individuals aged 12 and up.
Ontario also pledged to increase access to Paxlovid, an antiviral from Pfizer, which has been so far tough to access throughout Canada but can cut the risk of death when taken early in an infection.
“The most important thing is really focusing on, ‘What can I do to reduce my risk of severe infection should I get infected?’ And there you say, ‘OK, am I maximally vaccinated? And am I someone who should get tested early in case I’m eligible for a treatment?'” Saxinger said.
“And if you do get infected, rather than beating yourself up, make sure that you’re accessing all the available things that would be helpful.”
Article From: CBC News
Author: Adam Miller, Lauren Pelley

