COVID-19 vaccinations greatly reduce the risk of lasting respiratory and mental-health problems, but for many patients who got sick early in the pandemic, it’s too late. A difficult journey lies ahead for them
Laurel Schafer’s bedside nightstand is cluttered with the evidence of illness: an asthma inhaler to help her breathe; a beta blocker to keep her heart from racing when she stands; sleeping pills to stop the nightmares; painkillers to treat headaches; an anti-viral drug; a battalion of vitamins. A medical cocktail to fight Ms. Schafer’s lingering symptoms since COVID-19 sent the physically fit, then 35-year-old physiotherapist to bed last November in Swift Current, Sask.
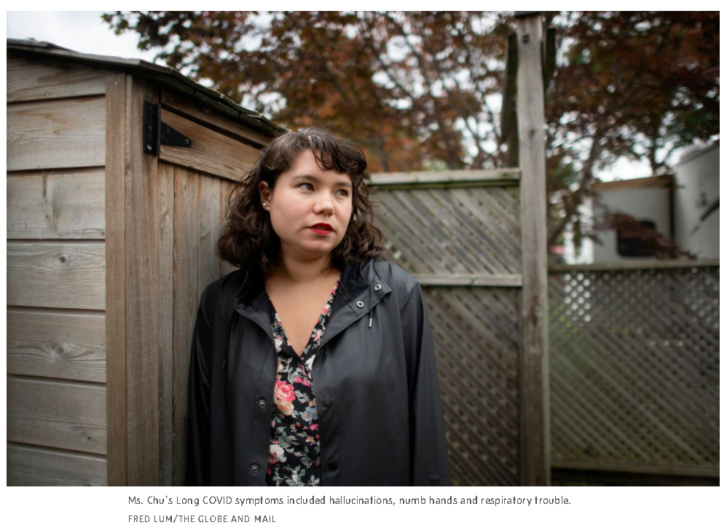
Leigh Ann Chu spent her 28th birthday in a Toronto emergency department receiving a psychiatric consult for depression, six months after a COVID-19 infection brought on hallucinations, made it impossible to work or play soccer, and eventually led to a broken engagement.

In Mirabel, Que., Valérie Murray, 37, used to run while pushing her lawn mower. Now, a year after she first experienced the symptoms of COVID-19, she uses a wheelchair, even in her house, and takes breaks while she eats because a spoon feels too heavy.
This is the continuing story behind the statistics of the pandemic’s“recovered cases.” According to conservative estimates, at least 10 per cent of Canadian adults infected by COVID-19 will have long-term, potentially debilitating symptoms, such as fatigue, brain fog, heart palpitations, trouble breathing and depression. That’s 165,000 Canadians, and rising, with the Delta variant spiking cases in provinces such as Alberta, Saskatchewan and New Brunswick.
As of now, there is no cure for what scientists are calling Post COVID-19 Condition, or Long COVID – only symptom management based on evolving science.
There is, however, a widely available prevention: getting vaccinated. A recent study out of Israel suggests that being vaccinated significantly reduces the risk of getting long-term symptoms, both by preventing infection in the first place and by improving outcomes for breakthrough cases. “It is agonizing to see something so preventable in a wealthy country like ours,” says Fahad Razak, an internist and epidemiologist at St. Michael’s Hospital, and the lead author of a recent Ontario Science Table paper on Long COVID.
While patients who end up in ICU are at higher risk, Long COVID happens even in mild cases, and among the young and healthy. (For example, although their cases are extreme, none of the women above were hospitalized during their acute COVID-19 infections.) A recent Lancet editorial declared Post COVID-19 Condition to be a “modern medical challenge of the first order.” It will further burden an already exhausted health care system. It will mean disability, absenteeism and stress for families.
And once again, it will hit certain households the hardest. The best treatment for the physical and mental-health symptoms of Long COVID includes occupational and physical therapists, as well as social workers and psychologists – the same care that many Canadians still have to pay for themselves, or else linger on wait lists for publicly funded services.
That’s a serious equity issue, especially since COVID-19 spread fastest among lower-income, precariously housed, tenuously employed and racialized Canadians, the least likely to have the resources or workplace benefits to get this kind of care.
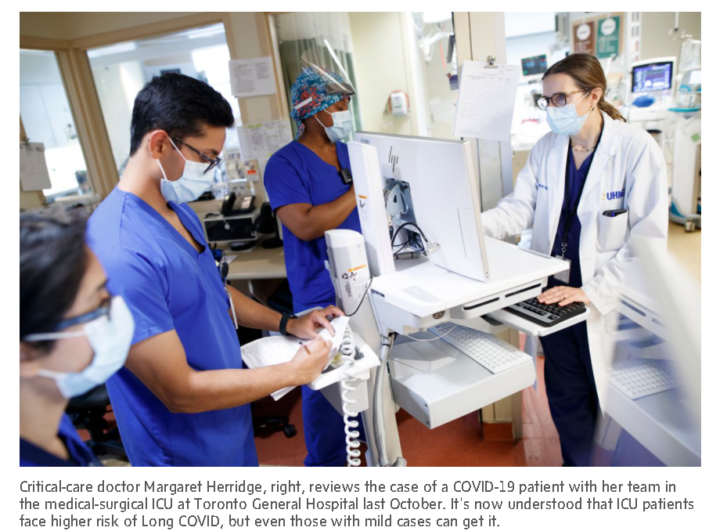
“Our system is really ill-equipped to deal with the enormous burden of illness that is becoming more apparent,” says Margaret Herridge, a critical-care specialist with Toronto’s University Health Network and the co-lead of CANCOV, a study collecting data on COVID-19 patients and their families. Her team, she says, will try to find treatment for vulnerable people in the study. “It can be a challenge, even for us.”
Already wait lists are growing at the country’s handful of Long COVID clinics. Dr. Razak says it is likely that more than 10 per cent of the infected population will have longer-term symptoms, although the severity will vary.
The World Health Organization estimated a rate of between 10 and 20 per cent, when it released an official definition of Post COVID-19 Condition this week. Other studies have suggested even higher rates, and since most research comes from early waves of the pandemic, the effect of the more virulent Delta variant is not known.
The early research also tends to include only people who actually tested positive for COVID-19. Ms. Chu, for instance, would not be in that group; she became sick early on when the virus was considered a mild risk for 20-somethings, and health workers were the testing priority, so her case was diagnosed based on her symptom history.
One lucky break, so far: Long-term symptoms also appear in children and teenagers, but studies estimate that only between 1 and 2 per cent of pediatric cases of COVID-19 lead to long-term symptoms, and those cases also appear to resolve more quickly than in adults.
“It can take months for some of these kids before they are feeling better,” but they generally improve, says Anu Wadhwa, an infectious-disease specialist at SickKids, who has treated patients as young as 5, although most of her cases involve teenagers.
In adult patients, having a higher body-mass index or an underlying health condition, being older and female appear to be risk factors, but researchers haven’t really figured out why some people are hit harder, or recover more slowly. “You just don’t know how the virus is going to react with your biology,” Dr. Herridge says.
Laurel Schafer, for instance, was active and healthy when her family was infected with COVID-19 last November. Her husband, who brought it home following a close contact at work, and her two children, 8 and 6, came down with relatively mild symptoms and then recovered.
But Ms. Schafer spent three weeks in bed, at one point with a headache so bad it hurt to move her eyeballs. She didn’t get a fever and she never fought for air, and she felt lucky to avoid the hospital.
When she continued to feel unwell, she thought that she could just “exercise her way out of it.” But that only made things worse.
Months later, her heart still races when she stands and she can barely muster the energy to chop vegetables for dinner. At night sometimes, she gets what she calls “flashy brain,” where it feels her head has an internal strobe light. The symptoms wax and wane, but most days she is in bed by early evening.
“I am basically being taken care of,” she says, of her family. “I get short of breath if I try to sit and fold a load of laundry.”
Yet, she looks at the situation in Saskatchewan, with cases rising rapidly around her, and many people still not taking precautions. “It is scary to me,” she says. “I want people to know that this is bad.”
The condition is often a diagnosis of exclusion, especially in the absence of a positive COVID-19 test – which requires lab work and imaging scans at backlogged hospitals to rule out other causes of heart trouble and dizziness.
Long COVID shares similarities to chronic fatigue syndrome, and some patients infected during the SARS outbreak almost two decades ago also developed longer-term side effects. But, according to the Ontario Science Table report, Post COVID-19 Condition has been associated with 10 organ systems and 200 symptoms. Fatigue is among the most common, but the list also includes hair loss and vomiting, and changes in taste and smell.
Early on in her illness, in the spring of 2020, Ms. Chu became so disturbed about tasting metal in her water that she fired off an angry letter to her landlord, baffling her then-fiancé. For the first four months,her symptoms ranged from difficult breathing and lung pain, to throwing up several times a week. She took a leave from her job as a cartographer and eventually left Kingston, where she was living with her boyfriend, and went to live with her parents in Toronto.
That summer, her sensory hallucinations continued – at times, she was convinced that her food had gone rotten; she would see a “silvery coating” of virus particles in her water glass – and she was diagnosed with post-viral psychosis. When she tried to play soccer, like the old days, her hands went numb, as if she was having a stroke.
She figures she went to emergency more than half a dozen times. One night, while trying to drive herself to the hospital in a familiar neighbourhood, she got lost for two hours. By her 28th birthday in June, she was barely leaving her room, worrying her parents so much they brought her to the hospital, concerned about her mental health.
“There was so much anxiety,” she remembers. “The doctors would be like, ‘I’m sorry, I can’t help you. I don’t know what to do with you.’”
In fact, it took an outspoken patient-advocacy movement, with a strong social-media presence, to get Long COVID recognized by the medical community. (It also helped that doctors and nurses infected by COVID-19 also reported symptoms that didn’t go away even after the acute infection period had passed.)
Anna Banerji, an infectious-disease specialist and pediatrician at St. Joseph’s Health Centre of Unity Health Toronto, was one of those health care workers. Eighteen months after contracting COVID-19 at work, food still tastes different, her full sense of smell has not returned, and she occasionally shakes with cold chills, even lying on a hot beach this summer.
A big part of the care she provides to patients with lingering symptoms, she says, is to tell them that she believes them, that she has heard their story before. “I see people who were athletes, hard workers,” she says. “The hardest thing for them is that people think they are just being lazy.”
Valérie Murray also never tested positive for COVID-19. But following a visit to the hospital for an allergic reaction in July, 2020, she lost her sense of taste and began to have trouble breathing and staying awake during the day. When she sought help, there were many theories: She had anxiety, allergies, reflux, an unknown virus.
Still sick by the end of the summer, she was sent to the Montreal Heart Institute, where she nearly fainted during a stress test on a treadmill. Finally, she felt, the doctors took her seriously. “It’s not in your head,” the specialist told her. The progression of her symptoms matched what they were learning about COVID-19′s long-term side effects.
“I started to cry,” she remembers. “It was a huge balm to my heart. I finally had a name for what I had.”
Still, knowing was not a cure. Today, the brain fog and exhaustion mean she cannot read for more than 15 minutes at a time. She struggles to find simple words. “Most of the time I have to wear sunglasses and earplugs because the overstimulation makes me even more exhausted.” Like Ms. Chu, she once got lost a couple of blocks from her house.
She feels grateful for her husband and kids, who have been resilient, but she says, “Our family life has been completely turned upside down.” The hardest part is managing the grief for what she can no longer do, and the uncertainty of not knowing if she will ever be her pre-COVID self again. “COVID is really sneaky: You never know which group you will fall into.”
Patients such as Ms. Murray are putting their hope in the research now being conducted around the world. On the treatment side, doctors suggest there is a learning opportunity here as well. “This is a condition that requires personalized attention,” Dr. Razak says. “You can’t diagnose this in a walk-in clinic.”
The only way to properly treat Long COVID, with its wide-ranging, highly variable symptoms, is with doctors from multiple specialties communicating as a team; with patients’ mental and physical health given due consideration; with rehabilitation as a focus.
Long COVID clinics are beginning to expand across the country. The rehab clinic at Providence Healthcare, part of Unity Health in Toronto, which offers virtual appointments with a team of specialists, has a growing wait list and a six-week wait for first appointments. Roughly 70 per cent of patients come from the community, as opposed to being referred out of ICU, says Ashley Verduyn, chief and director of medical affairs.
“This is an opportunity for something good to come from this tragedy,” Dr. Herridge says. Listening more to patients’ voices, understanding the need for individual care, collaborating to treat a patient’s mental and physical health. “It really should be a model of care that we take forward, and adopt and apply to all complex, complex cases.”
Meanwhile, the country is in the middle of the fourth wave and the virus continues to play out in people’s lives in diverse ways. While Ms. Murray and Ms. Schafer have continued to struggle with their symptoms, Leigh Ann Chu began to recover, a process she credits to the right medication, meditation and psychotherapy. Eight months after getting sick, she went back to work, although by then her relationship had ended.
She still gets numb hands sometimes when she plays soccer; she still has nightmares where she can’t breathe; and she is waiting for the results of a colonoscopy investigating continuing bowel issues. Not getting vaccinated, she says, is a gamble with your health and happiness.
“I considered myself a perfectly healthy person. I remember thinking, ‘It’s not going to happen to me,’” she said. “But it is going to happen to someone.”
Article From: Globe and Mail
Author: ERIN ANDERSSEN

