As we move into the third year of the global pandemic caused by COVID-19, it’s important to ask what we have learned and what we have done to prepare for the next infectious-disease crisis.
It could be an outbreak of Lyme disease, an epidemic of measles or another full-blown global pandemic of influenza or coronavirus. It could be a threat that emerges from the ongoing challenge of antimicrobial resistance and the steadily fading power of established antibiotics.
One thing is certain: COVID-19 will not be the last challenge of our time, and even while we are striving to tame the current pandemic, we need to prepare for the next challenge, using evidence and knowledge.
Infectious diseases
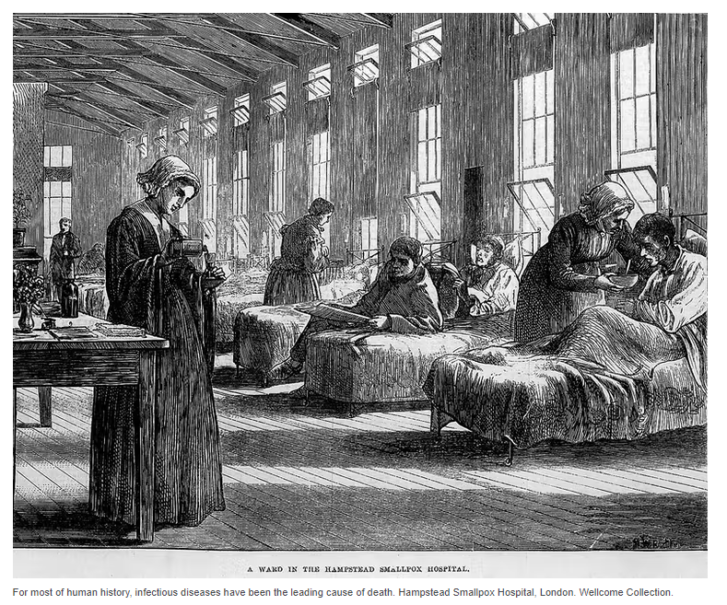
For most of human history, infectious diseases have been the leading cause of death, preying mainly on the very young, the old and the most vulnerable among us.
Scientific advancements in the 20th century reversed this historical trend — at least for a time.
Our ability to control infection through public health measures such as clean water and by developing vaccines, antibiotics, antiviral and antiparasitic agents has changed the way we live — and the way we die.
Statistics Canada data show that controlling infectious diseases has bought us more than two decades of extra life, on average. It’s a remarkable achievement, and as a result, diseases of aging — cancer, cardiovascular illness, chronic ailments, and degenerative neurological diseases such as Alzheimer’s — are now the major causes of death.
What we should have learned over the last few decades, however, is that our control over infection is illusory and that we remain vulnerable.
The 1970s saw the emergence of swine flu and Legionnaire’s disease. The ‘80s brought HIV/AIDS, the ’90s witnessed Ebola and the early 2000s brought the return of influenza with H1N1, the first SARS crisis and Middle East respiratory syndrome (MERS).
During that same period, the pharmaceutical industry put antibiotic discovery on the back burner, favouring the invention of more profitable treatments for chronic diseases, with their endlessly renewable prescriptions.
Without alternatives to penicillin, antimicrobial resistance has become, like climate change, a slow-moving but inexorably advancing global crisis.
Infection control
The current pandemic has forced governments, public health officials and the health-care sector overall into a prolonged emergency footing, showing us very clearly that we cannot take infection control for granted.

At the same time, we have been able to benefit from ongoing advancements in fundamental research and development. These advancements have enabled swift response to the current crisis with multiple vaccine platforms, do-it-yourself diagnostic tests featuring unprecedented sensitivity, new antiviral drugs and antibodies, and the real-time production of robust evidence and information to keep pace with every turn in the pandemic saga.
Information technology has developed with amazing speed, providing the opportunity to disseminate critical information instantly. The complete genome sequence of SARS-CoV-2, for example, was available to researchers across the globe well before the COVID-19 virus arrived on their doorsteps.
Still, this same technology has also provided a platform for those who would discredit these scientific advances, oppose public health sector leaders, and even interfere with front-line workers caring for patients.
One Health
Infectious diseases are almost always what we call One Health problems. The term refers to the intimate link between human and animal health, agriculture and the environment.
Microbes that cause disease often move easily between reservoirs in the environment, animals and people. Human encroachment into previously remote regions continues at an alarming rate, exposing us to previously isolated viruses, bacteria and parasites.
Climate change is creating new vectors to spread these diseases, such as ticks and mosquitoes migrating into newly warmed environments.
As climate change continues and the demand for nutrition grows, strains on the environment will generate new infection challenges. Seeing three unique, novel coronaviruses (SARS, MERS and SARS-CoV-2) jump from environmental reservoirs into humans in the space of a two decades should have spurred us to be vigilant, alert and prepared, yet we still aren’t ready enough.
Complacency
Public-health infrastructure, research into infectious diseases and the development of new therapies have been neglected for decades.
Before the pandemic, our increased lifespans and ability to neutralize some infections with preventions and treatments had lulled us into complacency regarding the infectious diseases we had once rightly feared.
With such easily accessible global travel and a standard of living that relies on international trade, turning back the clock is impossible.
We must anticipate and prepare for more outbreaks, epidemics and pandemics.
We need to establish robust research networks and be able to mobilize them quickly when new problems emerge.
We need to invest in biomedical and biomanufacturing infrastructure that can respond urgently to these challenges enabling us to rapidly produce new vaccines and drugs.
If we do not invest continuously in these platforms, we will doom ourselves to still more crises that we could have anticipated and prevented.
Article From: Conversation
Author: Gerry Wright, Professor of Biochemistry and Biomedical Sciences, McMaster University

