Case counts are soaring and hospitalizations are rising. But things are very different now than they were in March 2020.
Omicron has burst the New Year’s bubble. In Ontario, as students and teachers prepared to move returned to online learning online, Durham Region’s paramedic union revealed that the suburban area had posted multiple “Code Zeros,” meaning no ambulances were available, while Niagara Health is temporarily shuttering its Fort Erie urgent care centre because of the twin pressures of new admissions and staff shortages. In British Columbia, provincial health officer, Dr. Bonnie Henry, warned that businesses should prepare for the possibility that a third of their staff could be absent due to the virus and in St. John’s, outpatient appointments at its main rehabilitation hospital were cancelled due to an outbreak.
As case numbers continue to skyrocket, many of the basic restrictions first seen 22 months ago are coming back. But for those muttering that we’ve been thrown back to the beginning of this pandemic, experts point out that the situation is vastly different now thanks to vaccines, which for most people turn what can be a serious medical problem into a relatively mild illness.
Experts are hopeful that this will be a relatively short wave, because of what happened in South Africa, where Omicron was first detected. There, cases quickly spiked and then fell dramatically in around three weeks. But our trajectory is still unknown. Dr. Eileen De Villa, Toronto’s chief medical officer, warns that this wave may not peak for another four to six weeks, and the city is preparing to redeploy workers as needed to essential services. As infectious diseases physician Dr. Andrew Morris pointed out on The Agenda last night, Omicron is so new—it was declared a variant of concern on Nov. 26—and has spread around the world so quickly that everyone is together learning its behaviour in real time. “Virologists, molecular biologists, and epidemiologists are biting their nails and hoping cases will soon peak and begin to fall,” wrote Kai Kupferschmidt and Gretchen Vogel in Science. “They are also working at top speed to sort out the properties of the new variant.”
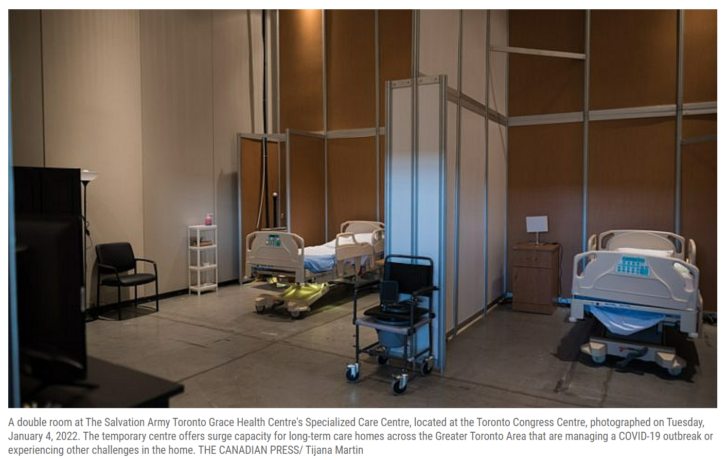
The big concern is our health care system. Though 82 per cent of Canadians have at least one dose of vaccine, that leaves nearly one-fifth of the population is unvaccinated. And with unprecedented numbers of COVID-19 infections—including a big spike in cases among seniors—that means the number of people eventually needing hospitalization could overwhelm the system. “What we’re seeing right now is just the beginning of a lagging effect of a massive increase in infections,” Morris said. The lag is showing up in the data: in the past 72 hours, some 124 new COVID-19 patients have been admitted to Ontario hospital critical care units, pushing the total to 284 while the province’s hospitalizations have jumped 115 per cent from a week ago.
We need to get through this wave. There are things that everyone can do to protect themselves and their communities.
The most obvious is to get vaccinated, with whichever dose is next for you: first, second or third. Dr. David Fisman, an epidemiologist at the University of Toronto, has a few more practical suggestions:
1. Get a proper respirator (N95 or equivalent) for you and your children. A close-fitting N95 mask—which filters air as you breathe it in—can offer significantly higher protection than surgical or cloth masks, even if it is not professionally fitted to a person’s face. The American Conference of Governmental Industrial Hygienists estimates it could take 25 hours for COVID-19 to transmit between people wearing N95 masks compared to 60 minutes if both use surgical masks and 27 minutes if both wear cloth masks. (It goes up to 2,500 hours for tightly sealed N95s, such as those worn by health care workers.)
2. Avoid indoor activities outside your social bubble, especially when people outside your immediate group are unmasked. (A social bubble is a small group and can include a neighbour or family of a child’s friend.)
3. For those who can, work remotely. If you need to work in person, or live in a setting with shared ventilation, then consider cracking a window if possible, or using/implementing air cleaners (ones with HEPA filters, which are now widely available, or a Corsi-Rosenthal box).
4. Take care of your physical health by staying active. Outdoor air is safe so bundle up to see friends, perhaps for a walk or skate.
5. Try to support independent businesses wherever possible. If you can afford it, splurge on take-out once in a while.
Article From: Maclean’s
Author: Patricia Treble

